Introduction
Varicose veins, a common vascular condition affecting a substantial portion of the adult population, are more than just swollen blood vessels. This comprehensive guide aims to provide an in-depth understanding of varicose veins, shedding light on their causes, symptoms, available treatments, preventive measures, and potential complications.
What Are Varicose Veins?
Varicose veins are characterized by the abnormal enlargement and twisting of blood vessels just beneath the skin’s surface, primarily occurring in the legs, feet, and ankles. These veins, often presenting as blue or purple bulges, can be accompanied by smaller, red or purple lines known as spider veins. While the aesthetic aspect is a concern, varicose veins can also induce discomfort, itching, and pain. Though not inherently dangerous, severe cases may lead to complications such as blood clots.

Varicose Veins vs. Spider Veins
| Feature | Varicose Veins | Spider Veins |
|---|---|---|
| Appearance | Swollen, twisted, bulging veins | Smaller, red or blue lines, resembling spider webs |
| Color | Blue or purple | Red or blue |
| Location | Legs, feet, ankles | Commonly on the face, behind the knee, or on feet |
| Size | Larger and more prominent | Smaller and thinner |
| Pain | Can be painful, achy, or sore | Typically not painful |
| Associated Symptoms | Heaviness, itching, swelling, skin discoloration | Often asymptomatic, may cause minor discomfort |
| Risk Factors | Age, gender, family history, lifestyle choices | Similar risk factors as varicose veins |
| Prevalence | Common, affecting around 1/3 of adults | Common, but prevalence may vary |
| Treatment | Elevation, compression stockings, medical procedures | Similar treatment options as varicose veins |

Exploring Risk Factors
Various factors contribute to the development of varicose veins, making it imperative to recognize and understand these risk elements. Age, gender, family history, lifestyle choices, overall health, tobacco use, and excess weight all play significant roles in increasing susceptibility to varicose veins. Awareness of these factors empowers individuals to adopt preventive measures and seek timely intervention.
Who is Likely to Get Varicose Veins?
Anyone can develop varicose veins. Certain factors increase your chances of developing varicose veins, including:
- Age: Because of the aging process, vein walls and valves don’t work as well as they once did. Veins lose elasticity and stiffen.
- Gender: Female hormones can allow the walls of the veins to stretch. People who are pregnant, taking the birth control pill or going through menopause have a higher risk of varicose veins because of changes in hormone levels.
- Family history: This condition can be inherited (runs in families).
- Lifestyle: Standing or sitting for long periods decreases circulation. Wearing restrictive clothing, such as girdles or pants with tight waistbands can decrease blood flow.
- Overall health: Certain health conditions, such as severe constipation or certain tumors, increase pressure in the veins.
- Tobacco use: People who use tobacco products are more likely to develop varicose veins.
- Weight: Excess weight puts pressure on blood vessels.

Symptoms
Identifying Symptoms
The most recognizable sign of varicose veins is a gnarled, blue or purple vein just under your skin’s surface. Symptoms include:
- Bulging veins: Twisted, swollen, rope-like veins are often blue or purple. They appear just below the surface of the skin on your legs, ankles and feet. They can develop in clusters. Tiny red or blue lines (spider veins) may appear nearby.
- Heavy legs: Muscles in your legs may feel tired, heavy or sluggish, especially after physical activity.
- Itching: The area around varicose veins may itch.
- Pain: Legs may be painful, achy or sore, especially behind your knees. You might have muscle cramps.
- Swelling: Your legs, ankles and feet can swell and throb.
- Skin discolorations and ulcers: If left untreated, varicose veins can cause brown discolorations on your skin. Severe varicose veins can cause venous ulcers (sores) on your skin.

Unraveling Causes
Varicose veins occur when the walls of your veins weaken. As blood pressure in your vein increases, the weakened walls allow your vein to get bigger. As your vein stretches, the valves that keep blood moving in one direction in your vein can’t work like they should. Sluggish blood backs up or pools in your vein, causing your vein to swell, bulge and twist.
Vein walls and valves can become weak for several reasons, including:
- Hormones.
- The aging process.
- Excess weight.
- Restrictive clothing.
- Pressure inside the vein from standing for long periods.

Image by: https://www.modernheartandvascular.com/venous-insufficiency-and-the-main-causes/
Diagnosis and Tests
Diagnosing varicose veins typically involves a physical examination. However, for a more detailed assessment and to check for potential complications, healthcare providers may recommend ultrasound imaging. This non-invasive procedure utilizes sound waves to produce images of internal tissues, providing valuable insights into the condition of blood clots and the functionality of valves within the veins.

Management and Treatment Options
Although there isn’t a cure for varicose veins, these treatments can reduce their appearance and relieve discomfort:
- Elevation: To increase blood flow and decrease pressure in your veins, you should elevate your legs above your waist several times throughout the day.
- Elastic stockings: Supportive stockings or socks compress your veins and reduce discomfort. The compression stops your veins from stretching and helps blood flow.
- Injection therapy (sclerotherapy): During sclerotherapy, a healthcare provider injects a solution into your vein. The solution causes the vein walls to stick together. Eventually, your vein turns into scar tissue and fades away.
- Laser therapy: In a minimally invasive procedure called endovenous thermal ablation, healthcare providers use a catheter (a long, thin tube) and laser to close off a damaged vein.
- Vein surgery: During these procedures, also called ligation and stripping, the surgeon ties off your affected vein (ligation) to stop blood from pooling. The surgeon may remove (strip) the vein to prevent varicose veins from reappearing.

Complications and Side Effects
Half of the people who have surgical stripping get varicose veins again within five years, and varicose veins can happen again after endovenous ablation as well.
Potential side effects of these treatments include:
- Scarring.
- Skin burns.
- Infection.
- Injury to a nerve.
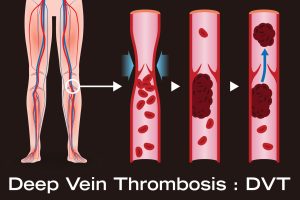
- Deep vein thrombosis (a blood clot in a vein deep inside your body).
Sclerotherapy can cause side effects that include:
- Redness or bruising for a few days where a needle went into your skin.
- Brown areas (for several months) on skin where the needle touched.
- Lumps or hardness for a few months.
With sclerotherapy, new varicose veins can happen and need treatment.
Prevention Strategies
You may not be able to prevent varicose veins. You can reduce your chances of developing them by living an active, healthy lifestyle. Healthcare providers recommend many of the same measures to prevent and treat varicose veins:
- Avoid long periods of standing: To encourage blood flow, take regular breaks to stretch and walk around, especially if you have a job that requires you to be on your feet.
- Elevate your legs: Raising your feet above your waist helps blood flow to your heart.
- Maintain a healthy weight: Getting rid of excess pounds reduces pressure inside your blood vessels.
- Quit tobacco use: Smoking damages blood vessels, decreases blood flow and causes a wide range of health problems.
- Stay active: To improve circulation, move frequently and avoid sitting still for prolonged periods.
- Try compression stockings: Support socks and pantyhose compress your veins and help blood circulate, which can prevent varicose veins from getting worse.
- Wear clothes that fit properly: To encourage blood flow, make sure your waistband isn’t too tight.
Outlook and Complications
Varicose veins can cause ulcers (open sores), bleeding and skin discoloration if left untreated. Severe varicose veins may be a sign of chronic venous insufficiency. This condition affects your veins’ ability to pump blood to your heart.
People who have varicose veins may be more likely to develop blood clots. It’s important to tell your healthcare provider about varicose veins. Your provider should evaluate and monitor you for clotting disorders such as:
- Superficial thrombophlebitis: Blood clots can form inside varicose veins, causing a condition called superficial venous thrombosis or superficial thrombophlebitis. Thrombophlebitis is painful but isn’t usually dangerous. It’s also treatable.
- Deep vein thrombosis (DVT): People with varicose veins have a higher risk of deep vein thrombosis, a blood clot in a vein deep inside your body.
- Pulmonary embolism: A blood clot in your body (usually resulting from DVT) can become lodged in your lung. Pulmonary embolism is a life-threatening condition that requires immediate treatment.

Conclusion
In conclusion, understanding varicose veins is pivotal for effective prevention and management. By recognizing symptoms, understanding risk factors, exploring available treatments, and adopting preventive measures, individuals can take proactive steps toward maintaining venous health and overall well-being. This comprehensive guide aims to empower readers with the knowledge needed to navigate the intricacies of varicose veins and make informed decisions about their vascular health.