Background
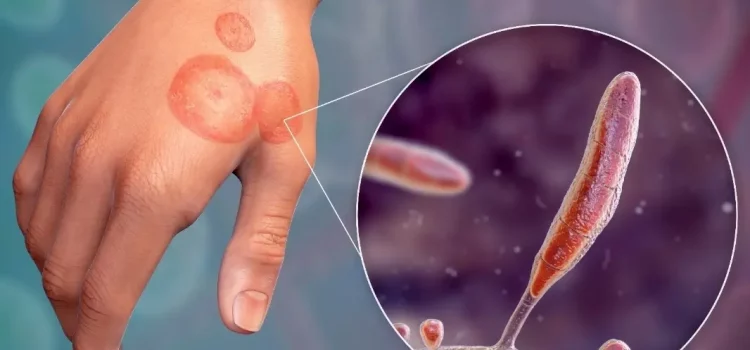
Antibiotic resistance poses a significant threat, particularly among vulnerable populations facing bacterial infections. In the realm of fungal diseases, such as those caused by C. neoformans, uncertainties persist regarding the role of host-derived factors. This study delves into the intricate dynamics of how host metabolites, notably glucose, influence the tolerance of C. neoformans to Amphotericin B (AmB), a critical fungicidal treatment.
Methodology
1. Sample Collection and Analysis
The study initiated with the collection of human cerebrospinal fluid (CSF) samples from patients afflicted with C. neoformans infection, with a primary focus on meningitis cases. The samples were subjected to analysis using high-performance anion-exchange chromatography (HPAEC) to quantify the levels of glucose, a metabolite of particular interest in this investigation.

2. Experimental Setup
Researchers designed a meticulous experimental framework to understand the dynamics of AmB tolerance concerning glucose levels. They tested the effectiveness of AmB on different strains in the presence of varying glucose concentrations. A single-cell-based method and time-series ribonucleic acid sequencing (RNA-seq) were employed to scrutinize the relationship between nuclear localization and Mig1-mediated AmB tolerance.
3. Additional Investigations
Beyond glucose, the study explored other factors influencing AmB tolerance. The role of Mig1, a fungal glucose repression activator, was examined after brain infection in mice. The impact of terbinafine, an ergosterol synthesis inhibitor, and inositol phosphorylceramide on AmB tolerance were also subjects of thorough investigation.
4. Animal Model and Treatments
Mice were enlisted as the animal model for evaluating the effectiveness of AmB coadministration versus monotherapy. To enhance drug access to the brain, a brain-targeting liposomal drug delivery strategy was adopted. The animals were sacrificed seven days after infection, and brain tissues were examined to assess fungal load and colony-forming units (c.f.u.).

Results
1. Glucose-Induced AmB Tolerance
- Glucose at brain-relevant concentrations significantly generated AmB tolerance.
- Galactose repression (GR) and the role of Mig1 in AmB tolerance were established.
2. Mig1-Mediated Tolerance Mechanism
- Mig1-regulated tolerance reduced therapy effectiveness by affecting ergosterol synthesis.
- AmB and aureobasidin A outperformed clinically indicated therapy against meningitis.
3. Metabolite Comparison
- Glucose, compared to other metabolites, caused higher AmB tolerance.
- Replacement of galactose with glucose mirrored survival percentages after AmB therapy.
4. Glucose-Dependent Tolerance
- Glucose-induced tolerance did not depend on macronutrient consumption.
- GOX and manganese dioxide therapy had varying impacts on AmB tolerance.
Conclusions
The comprehensive findings of this study underscore the pivotal role of glucose in fungal AmB resistance, mediated through the Mig1 glucose repression regulator. The identified Mig1-mediated brain glucose tolerance significantly diminishes the effectiveness of AmB treatment in rats. This study not only contributes to our understanding of AmB tolerance mechanisms but also points towards potential targets for adjuvant therapy. The intricate interplay between host-obtained metabolites and fungicidal tolerance revealed in this research opens new avenues for refining antifungal strategies, particularly in the context of cryptococcal meningitis treatment. As we delve deeper into the molecular intricacies, the study paves the way for future investigations and advancements in combating fungal infections.