The field of regenerative medicine has witnessed unprecedented advancements in recent years, promising to revolutionize healthcare by offering innovative solutions to previously intractable medical conditions. As we delve into the future of regenerative therapies, it is crucial to understand the current landscape, emerging technologies, and the potential implications for both patients and the medical community. This article explores the trajectory of regenerative therapies, focusing on key areas such as stem cell research, tissue engineering, and gene editing, while addressing the ethical and regulatory considerations that accompany these advancements.
Stem Cell Research: The Cornerstone of Regenerative Medicine
Stem cell research remains at the forefront of regenerative therapies, primarily due to the pluripotent nature of stem cells, which can differentiate into various cell types. This unique characteristic has made stem cells a cornerstone in the treatment of degenerative diseases, such as Parkinson’s, Alzheimer’s, and spinal cord injuries.
Recent breakthroughs in induced pluripotent stem cells (iPSCs) have opened new avenues for personalized medicine. iPSCs are derived from adult cells that have been reprogrammed to an embryonic-like state, thus bypassing the ethical concerns associated with embryonic stem cells. The ability to generate patient-specific iPSCs holds immense potential for developing tailored treatments, minimizing the risk of immune rejection, and enhancing therapeutic efficacy.

Tissue Engineering: Building Organs from Scratch
Tissue engineering is another critical component of regenerative therapies, aiming to create functional tissues and organs in the laboratory. The integration of biomaterials, cells, and bioactive molecules has led to the development of bioengineered tissues that can replace damaged or diseased tissues in patients.
One of the most promising advancements in this field is the development of 3D bioprinting technology. This innovative approach allows for the precise layering of cells and biomaterials to create complex tissue structures. Researchers have successfully bioprinted skin, cartilage, and even vascularized tissues, bringing us closer to the ultimate goal of printing fully functional organs.
The implications of tissue engineering are profound, particularly in addressing the shortage of donor organs for transplantation. Bioengineered organs could potentially eliminate the need for organ donors, reduce waiting times, and improve patient outcomes. However, significant challenges remain, including ensuring the long-term viability and functionality of engineered tissues and addressing the technical complexities of creating large, vascularized organs.
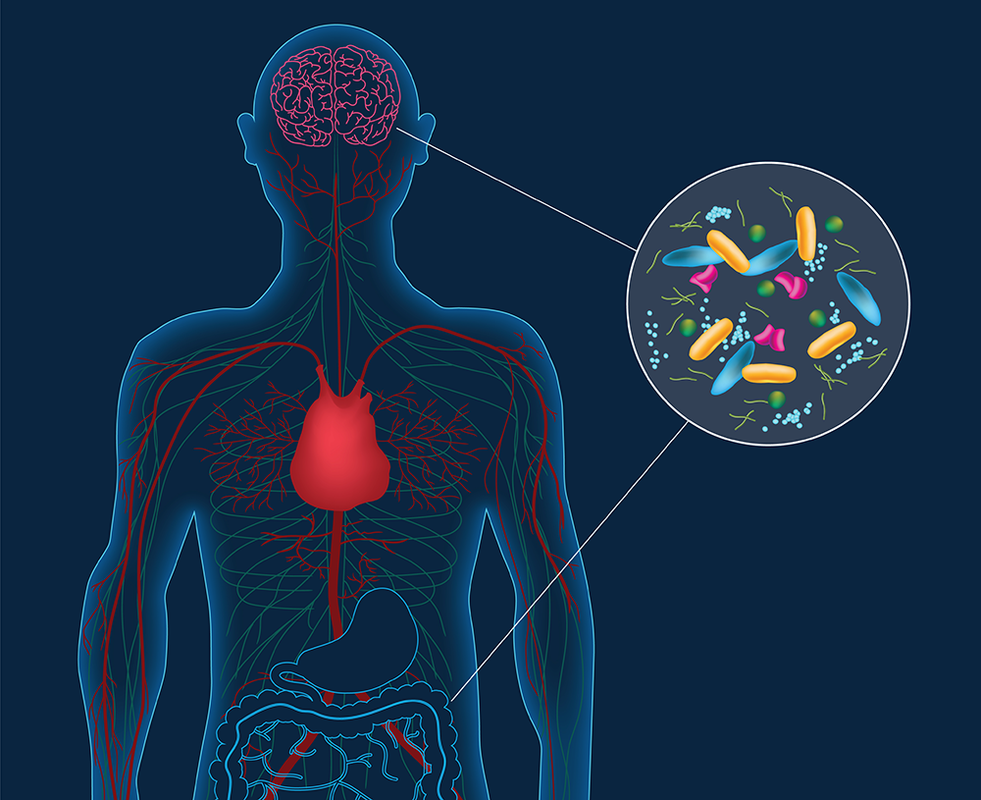
Gene Editing: Precision Medicine at Its Finest
Gene editing technologies, particularly CRISPR-Cas9, have garnered significant attention for their potential to correct genetic defects at the molecular level. This revolutionary tool allows for precise modifications to the genome, offering hope for the treatment of genetic disorders such as cystic fibrosis, muscular dystrophy, and sickle cell anemia.
The future of gene editing in regenerative therapies is promising, with ongoing research focused on improving the accuracy and efficiency of these techniques. Advances in delivery methods, such as viral vectors and nanoparticles, are enhancing the ability to target specific cells and tissues, minimizing off-target effects and increasing therapeutic potential.
Despite its promise, gene editing also raises ethical and regulatory concerns. The potential for germline editing, which involves changes to the DNA of embryos, poses significant ethical dilemmas, as these modifications would be heritable and could have unforeseen consequences for future generations. Regulatory frameworks must evolve to address these issues, ensuring that gene editing technologies are used responsibly and ethically.
Ethical and Regulatory Considerations
The rapid pace of advancements in regenerative therapies necessitates robust ethical and regulatory frameworks to ensure patient safety and the responsible use of these technologies. Ethical considerations include the sourcing of stem cells, the potential for genetic modifications, and the long-term implications of bioengineered tissues and organs.
Regulatory bodies, such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), play a crucial role in overseeing the development and approval of regenerative therapies. These agencies must balance the need for rigorous safety and efficacy standards with the urgency of bringing innovative treatments to patients. Streamlined regulatory pathways, such as the FDA’s Regenerative Medicine Advanced Therapy (RMAT) designation, are essential for accelerating the development and approval of promising therapies while maintaining high standards of patient safety.
The Road Ahead: Challenges and Opportunities
The future of regenerative therapies is undoubtedly bright, but several challenges must be addressed to realize their full potential. These include technical hurdles, such as improving the scalability and reproducibility of bioengineered tissues, and biological challenges, such as understanding the complex interactions between cells, biomaterials, and the host environment.
Collaboration between academia, industry, and regulatory bodies will be essential in overcoming these challenges. Public-private partnerships can facilitate the translation of scientific discoveries into clinical applications, while regulatory agencies can provide guidance and support to ensure the safe and effective development of new therapies.
Moreover, continued investment in research and development is critical. Funding from government agencies, private foundations, and industry partners will drive innovation and support the advancement of regenerative therapies. Education and training programs are also vital to equip the next generation of scientists, clinicians, and regulatory professionals with the skills and knowledge needed to navigate this rapidly evolving field.
Conclusion
Regenerative therapies hold the promise of transforming healthcare by offering novel solutions to some of the most challenging medical conditions. Advances in stem cell research, tissue engineering, and gene editing are paving the way for personalized, precision medicine that can restore function and improve quality of life for patients.
However, realizing the full potential of regenerative therapies will require addressing technical, ethical, and regulatory challenges. By fostering collaboration, investing in research, and developing robust regulatory frameworks, we can ensure that these groundbreaking therapies are developed responsibly and reach the patients who need them most.
As we look to the future, the continued evolution of regenerative therapies promises to redefine the boundaries of medicine, offering hope and healing to millions worldwide.