In the modern era, technology has permeated nearly every aspect of our lives, fundamentally transforming how we interact, work, and even manage our health. One of the most significant areas where technology has made a profound impact is in patient-doctor communication. This transformation has brought about both opportunities and challenges, reshaping the landscape of healthcare delivery in ways that were once unimaginable.
Evolution of Patient-Doctor Communication
Traditionally, patient-doctor communication was confined to face-to-face interactions within the clinical setting. Patients would schedule appointments, visit their healthcare providers, and discuss their symptoms and concerns in person. While this method allowed for direct and personal interaction, it also had limitations, such as accessibility issues, time constraints, and the potential for miscommunication due to the brief nature of consultations.
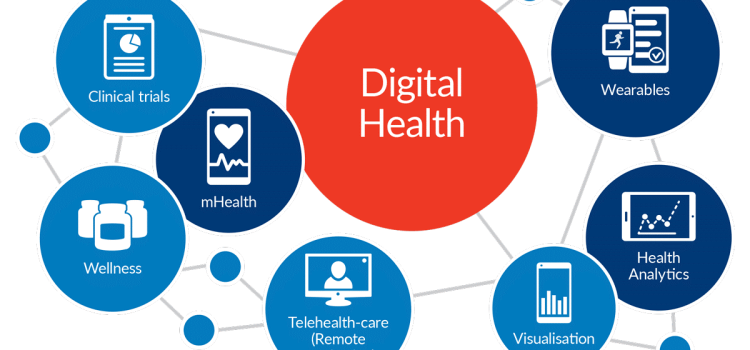
With the advent of technology, the dynamics of patient-doctor communication have undergone a significant shift. Digital tools and platforms have enabled more flexible, efficient, and continuous interactions between patients and healthcare providers. This evolution has been driven by several key technological advancements:
- Telemedicine and Virtual Consultations: Telemedicine has become a game-changer in patient-doctor communication. Through video calls, patients can consult with their doctors from the comfort of their homes, eliminating the need for travel and reducing wait times. This is particularly beneficial for individuals with mobility issues or those living in remote areas. Telemedicine also allows for more frequent check-ins, ensuring that patients receive timely medical advice and follow-up care.
- Electronic Health Records (EHRs): The digitization of health records has streamlined the sharing of patient information between healthcare providers. EHRs facilitate better coordination of care, as doctors can access a patient’s medical history, test results, and treatment plans in real-time. This comprehensive view enables more informed decision-making and enhances the overall quality of care.
- Patient Portals and Mobile Apps: Patient portals and mobile health apps have empowered patients to take a more active role in managing their health. These platforms allow patients to schedule appointments, request prescription refills, view test results, and communicate with their healthcare providers through secure messaging. By providing easy access to medical information and services, these tools enhance patient engagement and satisfaction.
- Wearable Devices and Remote Monitoring: Wearable devices, such as fitness trackers and smartwatches, have revolutionized the way health data is collected and monitored. These devices can track vital signs, physical activity, and even detect irregularities in real-time. Healthcare providers can remotely monitor patients’ health, enabling early intervention and personalized care plans. This continuous flow of data fosters a proactive approach to healthcare, shifting the focus from reactive treatment to preventive care.
Benefits of Technology-Enhanced Communication
The integration of technology into patient-doctor communication offers numerous benefits that contribute to improved healthcare outcomes:
- Accessibility and Convenience: Technology has made healthcare more accessible to a broader population. Patients no longer need to travel long distances or wait for extended periods to see a doctor. Virtual consultations and online services provide convenient options for those with busy schedules or limited mobility.
- Enhanced Patient Engagement: Digital tools empower patients to take control of their health. Access to medical records, educational resources, and personalized health recommendations fosters a sense of ownership and responsibility. Engaged patients are more likely to adhere to treatment plans, leading to better health outcomes.
- Improved Communication and Coordination: Technology facilitates seamless communication between patients and healthcare providers. Secure messaging platforms enable patients to ask questions, report symptoms, and receive timely responses. Additionally, EHRs and telemedicine platforms promote better coordination among healthcare teams, reducing the risk of errors and duplicative tests.
- Timely Interventions and Preventive Care: Remote monitoring and real-time data collection enable early detection of health issues. Healthcare providers can identify potential problems before they escalate, allowing for timely interventions. This proactive approach not only improves patient outcomes but also reduces healthcare costs by preventing complications and hospitalizations.
- Personalized Care: Technology allows for the customization of healthcare plans based on individual needs and preferences. Wearable devices and health apps provide valuable insights into a patient’s lifestyle and behavior, enabling tailored recommendations. Personalized care enhances patient satisfaction and adherence to treatment regimens.

Challenges and Considerations
While the benefits of technology in patient-doctor communication are undeniable, there are also challenges that need to be addressed:
- Privacy and Security: The digitalization of health information raises concerns about data privacy and security. Healthcare providers must implement robust measures to protect patient data from breaches and unauthorized access. Patients also need to be educated about the importance of safeguarding their personal health information.
- Digital Divide: Not all patients have equal access to technology. Socioeconomic factors, age, and digital literacy can create disparities in the adoption and use of digital health tools. Efforts must be made to bridge this digital divide and ensure that all patients can benefit from technological advancements.
- Quality of Communication: While virtual consultations offer convenience, they may lack the personal touch of in-person interactions. Non-verbal cues, such as body language and facial expressions, play a crucial role in communication and may be harder to interpret through digital platforms. Healthcare providers need to develop skills to effectively communicate and build rapport with patients in virtual settings.
- Technical Issues and Reliability: Technical glitches, such as poor internet connectivity or software malfunctions, can disrupt virtual consultations and hinder effective communication. Ensuring reliable and user-friendly technology is essential for maintaining the quality of care.
- Regulatory and Legal Considerations: The use of technology in healthcare is subject to regulatory and legal frameworks. Healthcare providers must navigate these regulations to ensure compliance and protect patient rights. Clear guidelines and standards are needed to govern the use of telemedicine, EHRs, and other digital health tools.
Conclusion
The impact of technology on patient-doctor communication is profound and multifaceted. By enhancing accessibility, engagement, and coordination, technology has the potential to revolutionize healthcare delivery and improve patient outcomes. However, it is essential to address the challenges and ensure that the benefits of technology are accessible to all patients. As technology continues to evolve, healthcare providers must embrace innovation while maintaining a patient-centered approach. By striking the right balance, we can harness the power of technology to create a more efficient, effective, and equitable healthcare system for all.