As we stand on the cusp of a new era in healthcare, genomic medicine is poised to revolutionize the way we understand, diagnose, and treat diseases. By 2025, the landscape of medicine is expected to be dramatically transformed by advancements in genomics, offering unprecedented insights into the human genome and paving the way for personalized medicine. This article explores the anticipated developments in genomic medicine by 2025, highlighting the key areas of progress and the potential impact on healthcare.
Understanding Genomic Medicine
Genomic medicine is a field that utilizes the information contained within an individual’s genome to guide clinical care. It involves the use of genomic information to predict disease risk, tailor treatments, and develop new therapies. The ultimate goal of genomic medicine is to provide personalized healthcare based on an individual’s genetic makeup.
Key Advances in Genomic Medicine by 2025
- Precision Medicine Becomes Mainstream
By 2025, precision medicine, which tailors medical treatment to the individual characteristics of each patient, is expected to become a standard practice in healthcare. This approach leverages genomic data to identify the most effective treatments for patients, minimizing adverse effects and optimizing therapeutic outcomes. Advances in genomic sequencing technologies and data analytics will play a crucial role in this transformation.
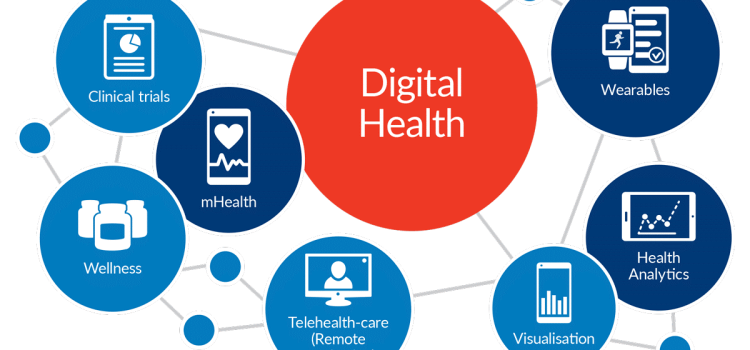
- Integration of Genomic Data into Electronic Health Records
The integration of genomic data into electronic health records (EHRs) is anticipated to be a significant milestone by 2025. This integration will enable healthcare providers to access comprehensive genetic information alongside traditional medical data, facilitating more informed decision-making and improving patient outcomes. The seamless incorporation of genomic data into EHRs will require robust data management systems and stringent privacy protections.
- Advancements in Gene Editing Technologies
Gene editing technologies, such as CRISPR-Cas9, are expected to witness substantial advancements by 2025. These technologies hold the potential to correct genetic mutations at their source, offering curative treatments for a range of genetic disorders. As our understanding of the human genome deepens, gene editing techniques will become more precise and efficient, opening new avenues for therapeutic interventions.
- Expanded Use of Polygenic Risk Scores
Polygenic risk scores, which assess an individual’s genetic predisposition to certain diseases based on multiple genetic variants, are likely to gain prominence by 2025. These scores will enable healthcare providers to identify individuals at high risk for conditions such as cardiovascular disease, diabetes, and cancer, allowing for early intervention and preventive measures. The widespread use of polygenic risk scores will necessitate advancements in computational tools and algorithms.
- Enhanced Understanding of Rare Genetic Disorders
The future of genomic medicine promises a deeper understanding of rare genetic disorders, many of which remain poorly understood today. By 2025, advancements in genomic research are expected to uncover the genetic basis of numerous rare diseases, facilitating the development of targeted therapies and improving diagnostic accuracy. Collaborative efforts between researchers, clinicians, and patients will be essential in driving these discoveries.
- Ethical and Regulatory Considerations
As genomic medicine continues to evolve, ethical and regulatory considerations will play a pivotal role in shaping its future. By 2025, frameworks for addressing issues such as genetic privacy, data security, and equitable access to genomic technologies will need to be established. Ensuring that genomic advancements benefit all segments of the population, regardless of socioeconomic status, will be a critical challenge for policymakers and healthcare providers.

The Impact on Healthcare
The anticipated advancements in genomic medicine by 2025 hold the potential to transform healthcare in several ways:
- Improved Disease Prevention and Early Detection
Genomic medicine will enable more accurate risk assessments for various diseases, allowing for targeted prevention strategies and early detection. This proactive approach to healthcare will reduce the burden of chronic diseases and improve overall population health.
- Personalized Treatment Plans
By harnessing the power of genomics, healthcare providers will be able to develop personalized treatment plans that consider an individual’s genetic makeup. This will lead to more effective therapies, reduced side effects, and improved patient satisfaction.
- Accelerated Drug Development
Genomic insights will facilitate the development of novel therapeutics by identifying new drug targets and enabling more efficient clinical trials. This will expedite the process of bringing new treatments to market, addressing unmet medical needs.
- Empowerment of Patients
Access to genomic information will empower patients to take an active role in their healthcare decisions. By understanding their genetic risks and predispositions, individuals can make informed lifestyle choices and collaborate with healthcare providers to manage their health proactively.
Challenges and Considerations
Despite the promising future of genomic medicine, several challenges and considerations must be addressed to realize its full potential:
- Data Management and Privacy
The integration of genomic data into healthcare systems will require robust data management solutions to ensure accuracy, security, and privacy. Establishing clear guidelines for data sharing and consent will be essential to protect patient information.
- Cost and Accessibility
Ensuring that genomic medicine is accessible to all individuals, regardless of socioeconomic status, will be a critical challenge. Efforts to reduce the cost of genomic sequencing and expand access to genomic services will be necessary to prevent disparities in healthcare.
- Education and Training
Healthcare providers will need to be equipped with the knowledge and skills to interpret and apply genomic information in clinical practice. Ongoing education and training programs will be essential to ensure that providers can effectively utilize genomic data to benefit patients.
Conclusion
The future of genomic medicine by 2025 holds immense promise for transforming healthcare and improving patient outcomes. As precision medicine becomes mainstream, advancements in gene editing technologies, polygenic risk scores, and the understanding of rare genetic disorders will drive progress in the field. However, addressing ethical, regulatory, and accessibility challenges will be crucial to ensure that the benefits of genomic medicine are realized by all. By embracing the potential of genomic medicine, we can usher in a new era of personalized, proactive, and patient-centered healthcare.








/cdn.vox-cdn.com/uploads/chorus_image/image/63243907/GettyImages_1126452706.0.jpg)