
Understanding Ovarian Cancer
Ovarian cancer, a condition characterized by the uncontrolled multiplication of cells in the ovaries, poses a significant health challenge for women. This article aims to provide a comprehensive overview, covering symptoms, types, risk factors, diagnosis, stages, treatment, ongoing research, prevention, and the outlook for those affected.
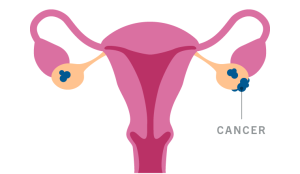
Ovarian Cancer at a Glance
The ovaries, crucial components of the female reproductive system, produce eggs and hormones such as estrogen and progesterone. Shockingly, around 19,880 women in the United States are estimated to receive an ovarian cancer diagnosis in 2022, with approximately 12,810 facing a tragic outcome.
Unveiling the Symptoms
Early Symptoms of Ovarian Cancer
Recognizing the early signs of ovarian cancer is crucial for timely intervention. While these symptoms can be subtle and easily dismissed, persistent occurrences warrant medical attention. Early symptoms may include:
- Abdominal Bloating, Pressure, and Pain: Unexplained sensations of fullness or discomfort in the abdominal area.
- Abnormal Fullness After Eating: Feeling excessively full or bloated after consuming small amounts of food.
- Difficulty Eating: Experiencing challenges or discomfort while eating.
- Increased Urination: An uptick in the frequency of urination without an apparent cause.
- Increased Urge to Urinate: A heightened sense of urgency to urinate, often unrelated to fluid intake.
It’s essential to note that these early symptoms may be indicative of various conditions, making their persistence and noticeable change from regular sensations significant for consultation with a healthcare professional.
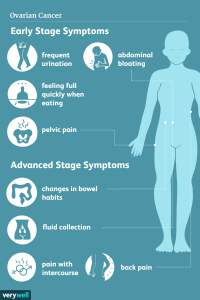
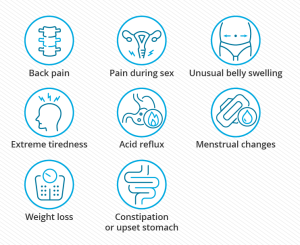
Later and Severe Symptoms
As ovarian cancer progresses, symptoms may become more pronounced and severe. These later signs often indicate advanced stages of the disease and may include:
- Fatigue: Persistent and unexplained tiredness or weakness.
- Indigestion: Discomfort or pain in the digestive system.
- Back Pain: Aching or discomfort in the back region.
- Menstrual Irregularities: Bleeding outside of the normal menstrual cycle.
- Painful Intercourse: Discomfort or pain during sexual activity.
- Dermatomyositis: A rare inflammatory disease leading to skin rash, muscle weakness, and inflamed muscles.
- Loss of Appetite: Decreased desire or interest in eating.
- Weight Loss: Unexplained and unintentional weight loss.
- Changes in Bowel Habits: Constipation or alterations in bowel movements.
Severe symptoms often signal the spread of cancer beyond the ovaries, making intervention more challenging.
Post-Menopausal Symptoms
Post-menopausal women should be vigilant about changes in their health, as ovarian cancer symptoms can vary after menopause. One key difference is the absence of regular menstrual periods. Post-menopausal symptoms may include:
- Bleeding After Menopause: Any unexpected bleeding after the cessation of regular menstrual periods should be investigated promptly.
- Persistent Abdominal Discomfort: Ongoing discomfort or pain in the abdominal area.
Post-menopausal women experiencing these symptoms should seek medical attention promptly, considering the potential association with ovarian cancer, which is more common in women over the age of 60.
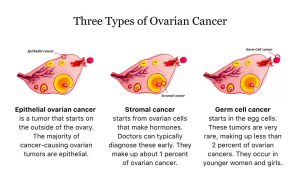
Types of Ovarian Cancer
Understanding the cellular origins is crucial:
- Epithelial Ovarian Carcinomas (85-90%): Form in the outer tissue layer.
- Stromal Tumors (7%): Develop in hormone-producing cells.
- Germ Cell Tumors: Rare, arising in egg-producing cells.
Ovarian Cysts: Benign vs. Cancerous
| Criteria | Benign Ovarian Cysts | Cancerous Ovarian Tumors |
|---|---|---|
| Composition | Typically filled with fluid | Solid masses of cells |
| Growth Patterns | May fluctuate in size with menstrual cycles | Do not exhibit growth or reduction with cycles |
| Post-Menopausal Occurrence | Uncommon | Occurrence may raise suspicion, requires evaluation |
| Symptoms | Often asymptomatic or mild symptoms | Can cause severe symptoms as they progress |
| Ovulation Association | Frequently associated with normal ovulation | Not linked to ovulation patterns |
| Detection Challenges | Usually detected incidentally during imaging | May require thorough evaluation and testing |
| Management Approach | Often monitored, may resolve on their own | May necessitate surgical intervention for removal |
| Cancer Possibility | Rarely associated with cancer | A small percentage can be cancerous, requiring careful assessment |
| Post-Menopausal Consideration | Typically less concerning | Requires careful evaluation due to increased cancer risk |
Risk Factors and Diagnosis
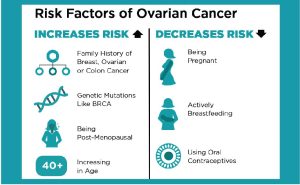
Risk Factors
- Family History:
- Presence of ovarian cancer in close relatives increases risk.
- Inherited genetic mutations (e.g., BRCA1, BRCA2) elevate susceptibility.
- Personal Cancer History:
- Previous breast, uterine, or colon cancer diagnosis raises risk.
- Age:
- Advanced age, especially post-menopausal, is a significant risk factor.
- Obesity:
- Higher body mass index (BMI) correlates with an increased risk.
- Fertility Treatments:
- Certain fertility drugs and hormone therapies may elevate risk.
- No History of Pregnancy:
- Women who have never been pregnant face a higher risk.
- Endometriosis:
- Presence of endometriosis increases the likelihood of ovarian cancer.
Diagnosis
Pelvic Exam:
Healthcare provider assesses pelvic abnormalities.
Transvaginal Ultrasound (TVUS):
Imaging test using sound waves to detect ovarian tumors.
CT Scan and MRI:
Cross-sectional imaging aids in evaluating spread and extent.
CA-125 Blood Test:
Measures cancer antigen levels; elevated levels may indicate ovarian cancer.
Biopsy:
Removal and analysis of a small tissue sample for definitive diagnosis.
Chest CT Scan and PET Scan:
Evaluates metastasis to lungs and distant organs.
Symptom Monitoring:
Persistent symptoms such as abdominal bloating prompt further investigation.
Genetic Testing:
Identification of genetic mutations associated with increased risk.
Clinical History Review:
Consideration of personal and family medical history.
Regular Check-ups:
Routine medical examinations for early detection and monitoring.

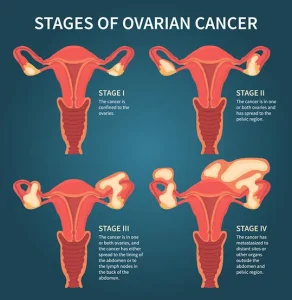
Navigating the Stages
The staging of ovarian cancer determines its spread:
- Stage 1: Limited to one ovary (1A) or both ovaries (1B), with possible external cell presence (1C).
- Stage 2: Involves spread to pelvic structures (2A, 2B).
- Stage 3: Spreads beyond the pelvis to abdominal lining and lymph nodes (3A, 3B, 3C).
- Stage 4: Metastasizes to distant organs (4A, 4B).
Treatment Approaches
A multidisciplinary approach is adopted based on the cancer’s extent. Common treatments include surgery (often involving hysterectomy), chemotherapy, targeted therapy, and hormone therapy. Fertility preservation options are explored for those seeking to conceive in the future.
Ongoing Research and Hope
The landscape of ovarian cancer research is dynamic, with constant exploration of novel therapies and treatments. Promising developments include PARP inhibitors, targeted therapies like navicixizumab and ATR inhibitors, gene therapies, and innovative clinical trials.
Prevention and Outlook
While complete prevention methods are elusive, factors like oral contraceptives, breastfeeding, pregnancy, and certain surgical procedures may lower ovarian cancer risk. The outlook depends on various factors, including cancer stage, overall health, and treatment response. Survival rates vary across stages, emphasizing the importance of early detection and intervention.
In summary, understanding ovarian cancer comprehensively empowers individuals, fostering awareness, early detection, and a hopeful outlook driven by continuous advancements in research and treatment modalities.










