

Introduction
Every January, healthcare providers and medical billers brace for changes to CPT codes. These codes—known as Current Procedural Terminology—drive billing, reimbursement, and compliance.
Staying informed on these changes is essential for accurate claims and optimal revenue cycles. In this guide, you will discover what CPT codes are and why they matter. You will get a clear overview of the 2025 updates, learn how to prepare your practice, and find tips for precise coding.
A summary table highlights the scope of changes. By the end, you’ll feel ready to navigate the new CPT landscape and keep your billing smooth.
What Are CPT Codes and Why They Matter
Role in Healthcare Billing
When providers submit claims, they attach CPT codes to describe services rendered. Accurate codes reduce denials and ensure you receive full payment. As medicine evolves, adding new codes and retiring obsolete ones keeps billing aligned with real-world clinical practice.
Why 2025 Updates Matter
The 2025 code set introduces the largest single-year expansion since 2021. According to the AMA, the book contains 270 new codes, 112 deletions, and 38 revisions, bringing the total change count to 420.
Nearly four in ten new entries cover proprietary laboratory analyses, many tied to advanced genetic tests. Ignoring these shifts can lead to down-coded claims, slower payments, and rejected prior authorizations.
What Is CPT?
The purpose of CPT codes
CPT stands for Current Procedural Terminology. These are five-digit numeric codes used by healthcare providers to describe medical, surgical, and diagnostic services. Insurers and government payers use CPT codes to process claims and set reimbursement rates. Accurate use of CPT codes ensures fair payment for services rendered and helps avoid audits and denials.
History of the CPT code set
The American Medical Association introduced CPT codes in 1966 to standardize billing across the United States. Over the decades, CPT has expanded to cover evolving medical technologies and treatments. Each year, the AMA’s CPT Editorial Panel reviews requests for new codes, revisions, and deletions. This process involves stakeholders from various specialties who ensure codes remain relevant and clear.
How the CPT Structure Works
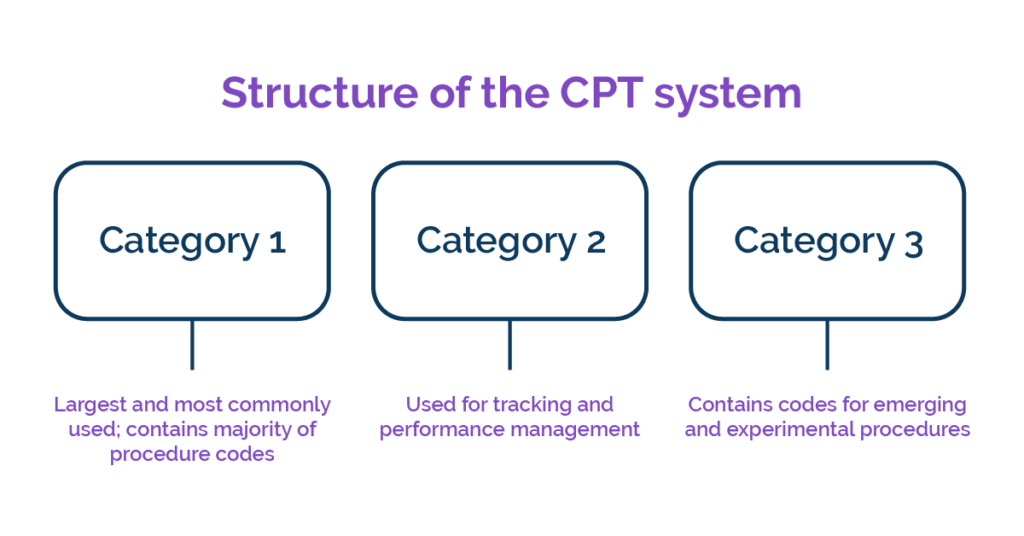
Category I
These permanent codes cover mainstream care such as office visits, vaccines, and common surgeries. Each code owns a unique descriptor and RVU value used by Medicare and most commercial payers.
Category II
Optional performance-measurement codes end in the letter F. They capture quality metrics—think blood-pressure checks—without affecting fee-for-service pay.
Category III
Temporary T-codes (ending in T) track experimental devices and procedures. A code can stay in Category III for up to five years; widespread adoption or supporting literature may promote it to Category I.
Key 2025 Highlights by Specialty
Primary Care and E/M
Nine new codes refine split/shared visit rules. Consistent templates reduce audit flags.
Telehealth and Remote Care
Medicine gains fresh codes for remote pulmonary rehab and extended RPM data review.
Laboratory and Genetics
Proprietary laboratory analyses dominate the additions list, reflecting payer appetite for precision oncology panels. Labs should cross-map internal test IDs to the new codes before January bills go out.
Surgery and Robotics
Minimally invasive endovascular repairs now have distinct add-on codes that capture robotic instrument use. Clear descriptors help surgeons prove clinical value and win fair payments for capital-heavy technology.
Linking CPT With ICD-10 and HCPCS
A CPT code tells insurers what was done, but a claim also needs an ICD-10 diagnosis to explain why. Pairing must satisfy payer policies and National Correct Coding edits. Some supplies—like durable medical equipment—require separate HCPCS Level II codes. Billing software that auto-checks links reduces denials.
Documentation Tips for a Clean Claim
Good notes are the backbone of coding accuracy. Follow these steps:
- Capture medical necessity early. A clear chief complaint and objective findings justify most procedures.
- List time spent. Many 2025 E/M selections hinge on total clinician minutes, especially for prolonged services.
- State technology specifics. For AI-assisted imaging or digital therapy, note the brand and algorithm version to align with Category III descriptors.
- Keep labs traceable. Record specimen source, methodology, and any proprietary test name to defend specialized PLAs.
Training Your Team
Coders, billers, and front-desk staff need role-specific refreshers each fall. Short weekly micro-learning modules beat marathon seminars. Pair lessons with real charts from your EHR sandbox so learners see mistakes in context. For deep dives, the AMA’s CPT QuickRef app and AAPC webinars remain gold standards.
How to Prepare for 2025 CPT Changes
Update billing software and tools
Ensure your practice management and coding systems receive the 2025 CPT code set before the effective date. Many vendors push automatic updates. If you manage updates manually, download the AMA’s digital files and import them into your system.
Train your billing and coding staff
Hold training sessions on major code changes and new definitions. Use AMA webinars, coding association courses, and specialty society guides. Give real-world examples of when new codes apply and how to sequence services.
Audit current coding practices
Perform internal audits of recent claims to identify reliance on codes slated for deletion. Review areas with high denials related to remote monitoring or genetic testing. Correct any use of outdated codes and refile claims where needed.
Communicate changes to clinical teams
Physicians and mid-level providers must know which services require new CPT codes. Share cheat sheets that map old codes to new ones. Encourage clinicians to document time, technology used, and medical necessity clearly to support correct coding.
Technology Tools to Speed Adoption

Computer-Assisted Coding
Natural-language engines scan notes and suggest possible codes, cutting manual lookup time. Be sure the engine’s 2025 dictionary lands in your test environment by November for parallel runs.
Insurance Contract Considerations
Commercial payers often lag on fee schedule refreshes. Before January 1, send a notice requesting updated reimbursement rates for every new Category I code you will report. For Category III items, negotiate case-rate pilots tied to outcomes rather than volume.Future Outlook
Conclusion
Learning the structure, updating templates, and aligning documentation now will prevent denied claims and protect revenue. Equip your team with up-to-date tools, establish weekly denial reviews, and open talks with payers early. By mastering the new codes before they activate, you ensure smoother cash flow and better patient access to cutting-edge care.
Call to Action: Download our free CPT 2025 Transition Checklist to map old codes to new ones, track payer updates, and train your staff before January 1—keep your revenue cycle running without a hitch.









