Introduction
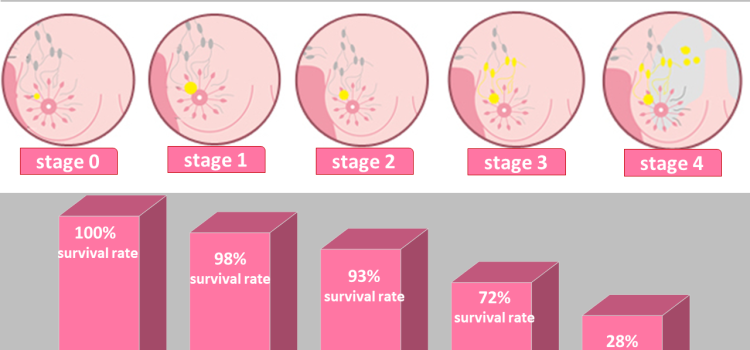
Understanding breast cancer stages is key to choosing the right treatment and predicting outcomes. When doctors talk about staging breast cancer, they refer to how far the cancer has spread in the body. Each breast cancer stage has specific features—tumor size, lymph node involvement, and whether it has metastasized. In this expert analysis, we’ll break down stages 0 through IV in simple terms. You’ll learn what tests doctors use, what each stage means for you or a loved one, and why early detection is so important.
What Is Breast Cancer Staging?
Staging is a way to describe cancer’s size and spread. It uses a system called TNM:
- T (Tumor): Size of the main tumor (T0–T4).
- N (Nodes): Whether cancer has reached nearby lymph nodes (N0–N3).
- M (Metastasis): Whether cancer has spread to distant organs (M0 or M1).
After assessing TNM, doctors assign an overall stage:
- Stage 0 (carcinoma in situ)
- Stage I (early)
- Stage II (locally advanced)
- Stage III (more locally advanced)
- Stage IV (metastatic)
Staging helps oncologists design personalized treatments. It also allows patients to understand prognosis and connect with support resources.
Stage 0: Carcinoma In Situ
Stage 0 is the earliest form of breast cancer. Here, abnormal cells reside in the ducts or lobules but have not invaded nearby tissue. Two main types:
- Ductal Carcinoma In Situ (DCIS): Cancer cells in the milk ducts.
- Lobular Carcinoma In Situ (LCIS): Abnormal cells in the lobules.
Key Points
- Tumor is non-invasive (Tis).
- No lymph node involvement (N0).
- No metastasis (M0).
Diagnosis and Treatment
- Diagnosis: Often found on mammograms.
- Treatment: Surgery (lumpectomy or mastectomy) plus radiation.
- Hormone Therapy: May follow if cells are hormone-receptor positive.
Stage 0 has an excellent prognosis—near-100 percent five-year survival—when treated promptly.
Stage I: Early Invasive Cancer
Stage I is the first invasive stage. Cancer cells have begun to spread into nearby breast tissue but remain small.
Substages
- Stage IA: Tumor ≤ 2 cm (T1), no lymph nodes (N0), no metastasis (M0).
- Stage IB: Small clusters (0.2–2 mm) of cancer cells in lymph nodes (N1mi), tumor ≤ 2 cm (T1), no metastasis (M0).
Diagnosis and Treatment
- Imaging: Mammogram, ultrasound, MRI.
- Biopsy: Core needle or surgical.
- Surgery: Lumpectomy with sentinel node biopsy or mastectomy.
- Radiation Therapy: After lumpectomy.
- Systemic Therapy:
- Chemotherapy: Based on tumor grade and biomarkers.
- Hormone Therapy: For estrogen/progesterone-receptor positive tumors.
- Targeted Therapy: Trastuzumab for HER2 positive cases.
Five-year survival rates exceed 90 percent for stage I.
Stage II: Locally Advanced
Stage II cancers are larger or have spread to a few nearby lymph nodes.
Substages
- Stage IIA:
- T0–T1 tumor (≤ 2 cm) with cancer in 1–3 axillary nodes (N1), or
- T2 tumor (2–5 cm) with no nodes (N0).
- Stage IIB:
- T2 tumor (2–5 cm) with 1–3 nodes (N1), or
- T3 tumor (> 5 cm) with no nodes (N0).
Diagnosis and Treatment
- Imaging: Breast MRI to check for multifocal disease.
- Surgery: Lumpectomy plus axillary node dissection or mastectomy.
- Radiation: Standard after breast-conserving surgery; chest wall irradiation for mastectomy with nodes.
- Systemic Therapy:
- Chemotherapy: Often recommended for stage II.
- Hormone Therapy: For receptor-positive.
- Targeted Therapy: HER2-directed agents as needed.
Five-year survival drops to around 80–90 percent but varies by subtype and treatment response.
Stage III: More Advanced Local Disease
Stage III is divided into IIIA, IIIB, and IIIC—reflecting greater tumor size, node involvement, or chest wall invasion, but no distant spread.
Stage IIIA
- Tumor: Up to T3 (> 5 cm).
- Nodes: 1–3 positive and level I–II nodes, or 4–9 nodes (N2).
Stage IIIB
- Tumor: Any size with direct extension to chest wall or skin (T4).
- Nodes: Any N0–N2.
Stage IIIC
- Tumor: Any size (T0–T4).
- Nodes: ≥ 10 positive axillary nodes (N3).
Diagnosis and Treatment
- Systemic Therapy First: Neoadjuvant chemotherapy to shrink tumors.
- Surgery: Modified radical mastectomy or breast-conserving with axillary clearance if downstaged.
- Radiation: After surgery to chest wall and regional nodes.
- Additional Therapies:
- Hormone Therapy and Targeted Therapy based on biomarkers.
- Clinical Trials: Emerging immunotherapy and PARP inhibitors.
Survival rates vary widely—stage IIIA around 72 percent, IIIB ~65 percent, IIIC ~49 percent five-year survival.
Stage IV: Metastatic Breast Cancer
Stage IV, or metastatic breast cancer, means cancer has spread beyond breast and local nodes to distant organs, such as bones, liver, lungs, or brain.
Characteristics
- Any Tumor Size (T0–T4)
- Any Node Status (N0–N3)
- Distant Metastasis (M1)
Diagnosis and Treatment
- Imaging: PET-CT, bone scans, MRI of brain (if indicated).
- Biopsy: Of a metastatic site to confirm diagnosis and test biomarkers.
- Systemic Therapies:
- Hormone Therapy: For receptor-positive disease.
- Chemotherapy: For visceral crisis or hormone-resistant cases.
- Targeted Agents: CDK4/6 inhibitors, HER2-directed therapy, PARP inhibitors for BRCA mutations.
- Immunotherapy: For PD-L1 positive triple-negative breast cancer.
- Palliative Care: Radiation to relieve pain, surgery for complications.
While not curable, many patients live years with stage IV cancer. Median survival has improved to 3–5 years or more, depending on subtype and treatment advances.
Special Considerations in Staging
Several factors refine staging and treatment:
Biomarker Status
- Hormone Receptor (HR) Positive vs. Negative
- HER2 Positive vs. Negative
- Triple-Negative
- Ki-67 Proliferation Index
These markers guide specific targeted therapies and influence prognosis.
Genetic Testing
- BRCA1/2 and Other Mutations: Inform risk of recurrence, eligibility for PARP inhibitors, and preventive measures for relatives.
Multigene Assays
Tests like Oncotype DX score risk of recurrence and chemo benefit in early HR positive, HER2 negative cancers. This helps avoid overtreatment.
The Importance of Early Detection
Early stages (0–I) offer the best outcomes. Key strategies include:
- Regular Mammograms: Starting at age 40–50 per guidelines.
- Self-Exams and Clinical Exams: Monthly checks and annual doctor visits.
- High-Risk Screening: MRI for those with genetic risk or strong family history.
Raising awareness and improving access to screening can shift diagnoses toward early, highly treatable stages.
Living with Each Stage
Support needs differ by stage:
- Stages 0–I: Focus on recovery, body image, and returning to work.
- Stages II–III: Manage treatment side effects, fatigue, and emotional stress.
- Stage IV: Emphasis on symptom control, quality of life, and palliative support.
Resources include counseling, support groups, rehabilitation programs, and survivorship care plans.
Conclusion
Decoding the stages of breast cancer helps patients and caregivers navigate treatment choices and understand prognosis. From non-invasive Stage 0 to metastatic Stage IV, each phase demands targeted strategies. Advances in staging—TNM classification, biomarker testing, and genetic profiling—allow personalized care that improves survival and quality of life. Early detection remains vital to catch cancers in their most treatable stages. As research continues, new therapies and precision medicine promise even better outcomes. By learning about breast cancer staging and seeking timely care, individuals can face this journey with knowledge, hope, and expert-backed guidance.